Test Results
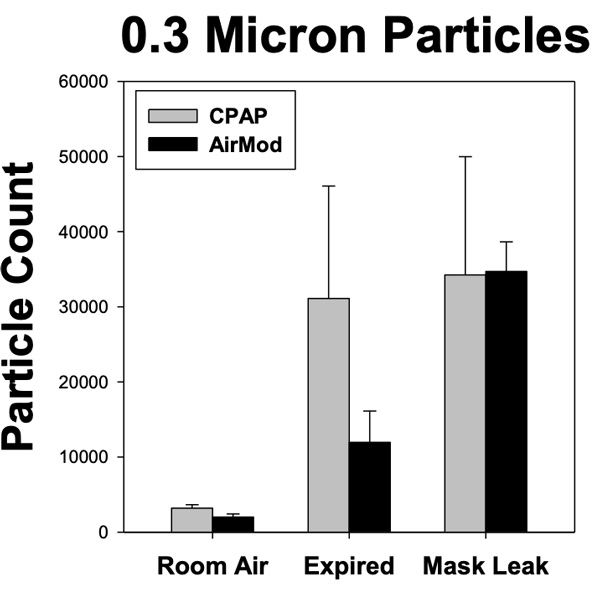
To examine the effect of the NYU Tandon AirMOD on spread of small particles around the patient, we used a nebulizer with a saline solution to create a large number of small particles that could be inspired and tracked in the expired air. The AirMOD represents the modification of the CPAP air circuit so expired air goes through a viral filter before entering the room air around the patient. We used a particle counter to measure the 0.3 micron particles in the expired air to determine the particle spread. Figure 1 demonstrates the results of two tests, one with a regular CPAP mask without any filter and the other using the AirMOD to filter the virus out of the expired air. Figure 1 demonstrates that the number of 0.3 micron particles were ~3,000 in the room air over a 5 sec sample. When sampling from expired air around the CPAP mask we found the particles increased to ~30,000. In contrast, the AirMOD was able to filter out ~60% of the particles. The AirMOD was even more effective with larger particles reducing particles from 0.5-10 microns by 82-88%.
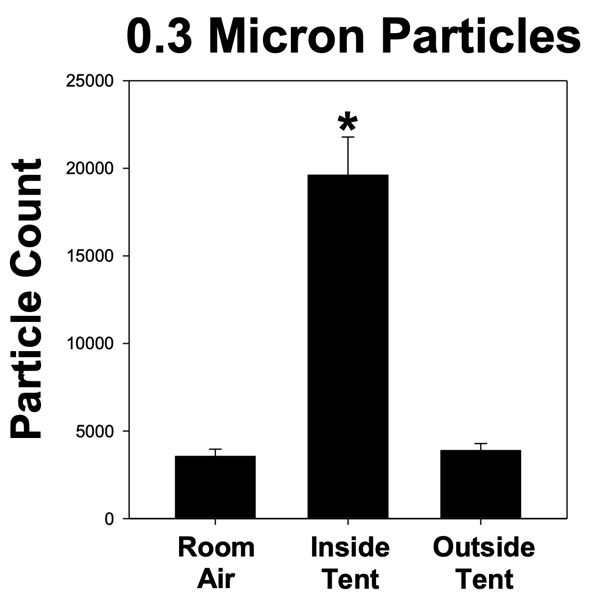
To examine the effectiveness of the NYU Tandon AirVENT system to minimize the spread of small particles, we measured the 0.3-10 micron particles within the mobile isolation tent created by the AirVENT as well as levels in the outside room air. Figure 2 demonstrates the AirVENT setup using the salon hood to create negative air flow attached to six clear plastic sheets to create a personal negative pressure tent. The tent is not sealed and provides easy access to the patient and relies on the negative air flow into the tent to ensure expired particles containing the COVID-19 virus are taken up by airflow through hood and into HEPA filter. In addition, the tent is big enough that patients can eat and talk to health care providers.
Figure 3 demonstrates that baseline room air levels of 0.3 microns were mean of 3549 particles from 5 second samples. Having Dr. Serrador breathe in the nebulized saline and expire into the AirVENT isolation tent resulted in an increase in 0.3 micron particles to 19,601 within the air inside the tent. However, these increased particles did not spread outside the tent as can be seen in Figure 3 since the outside air tent particle count remained at 3,884 particles. In fact, based on these numbers, there were an additional 16,052 particles added to the air inside the tent over the baseline level. The AirVENT was able to clear 15,717 particles resulting in only an increase of 335 particles in the area outside the tent. This represents a clearance of 98% of these particles by the AirVENT. Examining larger particles of 0.5-10 microns, clearance levels ranged from 95-100%.
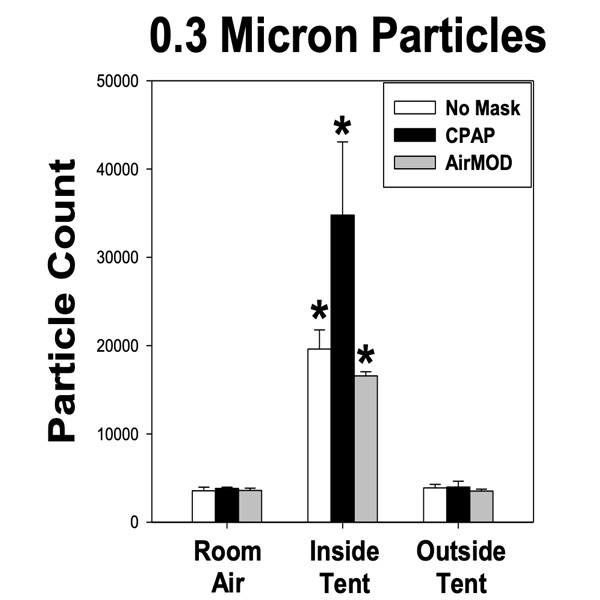
Examining how using the AirVENT system reduces particle spread in individuals using either regular CPAP or the AirMOD system demonstrated a similar ability to limit spread. Figure 4 demonstrates that while baseline particle count during each trial were ~3000, this count increased dramatically when nebulized droplets were added to the inspired air, indicated by the ~20,000-35,000 counts found in the air inside the tent. As can be seen, the standard CPAP mask increased the number of particles within the tent, a concern for use of CPAP with COVID-19 patients. In contrast the AirMOD slightly reduced the number of particle within the tent. With the use of the AirVENT system, particle count was close to room air outside the tent, regardless of the mask. In fact, while counts were reduced 98% in the no mask and CPAP mask conditions, the count returned to baseline levels in the condition where the AirVENT was used with the AirMOD, indicating that 100% of the particles were able to be contained.


Dr. Serrador obtained a particle meter from Grainger to determine the efficacy of AirVENT in scavenging 0.3 micron particles. For baseline measurements, he determined that the room where the test was being conducted yielded a count of approximately 2K for 0.3 micron particles. Next, a fog machine was placed inside the AirVENT tent to add lots of 0.3 micron particles. This yielded a count of approximately 20K for 0.3 micron particles inside the tent. With the AirVENT off, the 0.3 micron particle count outside the AirVENT tent increased to approximately 10K. When the AirVENT was turned on, the 0.3 micron particle count outside the AirVENT tent dropped down and returned to the baseline value of approximately 2K. This illustrates the efficacy of the AirVENT fitted with a HEPA-grade filter in scavenging the 0.3 micron particles.

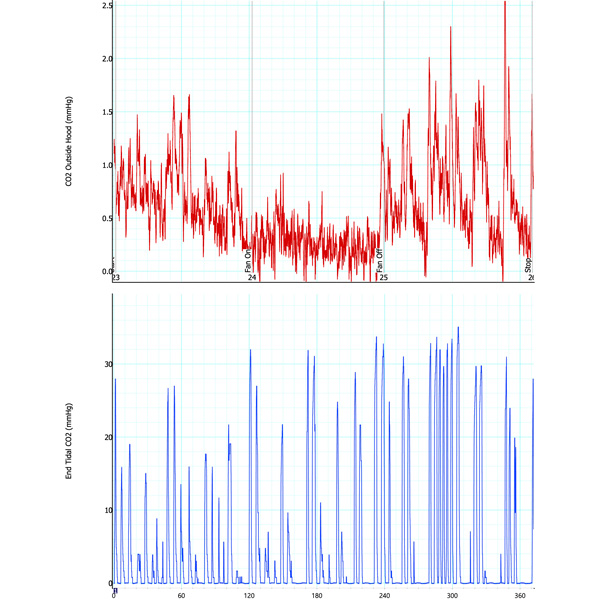
Similar to the tests with home-brewed negative pressure hood, measurements were done with the salon dryer negative pressure hood, i.e., the AirVENT. In this case, measurements were done (1) when the experimenter did not wear AirMOD (i.e., CPAP) and (2) when the experimenter wore the AirMOD. The corresponding results for the expired CO2 measurements inside the AirVENT (by the experimenter’s nose) and outside the AirVENT are given in two plots below. From each plot, it is seen that the expired CO2 measurements outside the AirVENT drop significantly when the AirVENT is turned on, illustrating the efficacy of the device to scavenge expired CO2. This demonstrates that the device can be a suitable tool in containing the spread of the aerosolized virus by a COVID-19 patient.
Attached is a screen shot of one test showing the effectiveness of the hood to scavenge expired CO2. The top panel in the graph shows CO2 levels being measured from just outside the hood. The lower panel in the graph shows the CO2 being sampled at the experimenter’s (Dr. Serrador) nose, i.e., in the exhale. The first 90 seconds (horizontal axis units in seconds) shows measurements with the fan of the negative pressure hood off. In the lower panel of the graph, the expired CO2 peaked at about 36-38 mmHg (~5%), which is considered normal. The peaks outside the hood were ~3-4 mmHg (top graph) or ~10% of the expired breath. This is a substantial amount of molecules (~1.3x1017). At ~95 seconds the fan of the hood was turned on. As seen in the lower panel of the graph, the turning on of the hood fan did not affect the amount of CO2 being exhaled out. However, the peaks completely disappeared in the upper graph indicating that the CO2 was no longer present outside the hood and that this negative pressure hood was effectively scavenging the expired CO2. At ~250 sec the fan was turned off and then the CO2 can be seen peaking outside the hood (top graph) return.
The two peaks in the middle of the graph on tops panel occurred when experimenter leaned out of the hood a little bit to answer some questions from his brand new research assistant (Dr. Serrador’s wife Jen assumed the role of his research assistant as the project is being conducted during the Covid-19 shelter in place order!).